Over the past few weeks we have seen COVID-19 numbers increase in Georgia and exponentially in Bulloch County. Grice Connect has received many questions from our readers regarding this spike and COVID-19. We picked questions we have received the most and reached out today to Jeffery A. Jones, Ph.D., Associate Professor, Department of Health Policy and Community Health, Jiann-Ping Hsu College of Public Health at Georgia Southern University to help us walk through these questions from a local perspective.
The questions I presented to Dr. Jones are in bold. What follows is his reply to each question. We hope this helps to tone down some misinformation and confusion surrounding COVID-19 and it’s continued impact on Bulloch County.
With COVID-19 positives increasing over 90%, or 104 cases, in one week in Bulloch County, hospital admissions trending up and with the age of positives trending down, when should citizens become concerned?
Dr. Jeffery Jones: “My answer is more an opinion as someone in public health. I believe that all Georgians should be concerned starting as far back as March 3rd when the first confirmed case was reported in our state. COVID-19 is new. None of us started this pandemic with immunity. We have known for months that this virus has some frightening properties. It can spread through the air from things as joyful as singing in a choir. People can have no symptoms for days …or at all…and be unknowingly infecting their loved ones and community. There is no vaccine currently and very limited treatments. As we have seen in Albany in March and in other clusters around the world (nursing homes, meat-packing plants, church choirs), outbreaks can occur among a roomful of people and quickly explode into hundreds of infected individuals. Sadly, until there is a vaccine or comprehensive treatment for this disease, we must remain concerned regardless of ups and downs in the numbers. A low number in cases one day can become a very different story in a week.”
Many in our community are attributing higher positives to more testing. However, our positive test percentages are around 10% with an infection rate of 1.06%. We are definitely seeing a rapid spread of COVID-19. Can you give us your thoughts on where we are with positives in relation to increased testing?
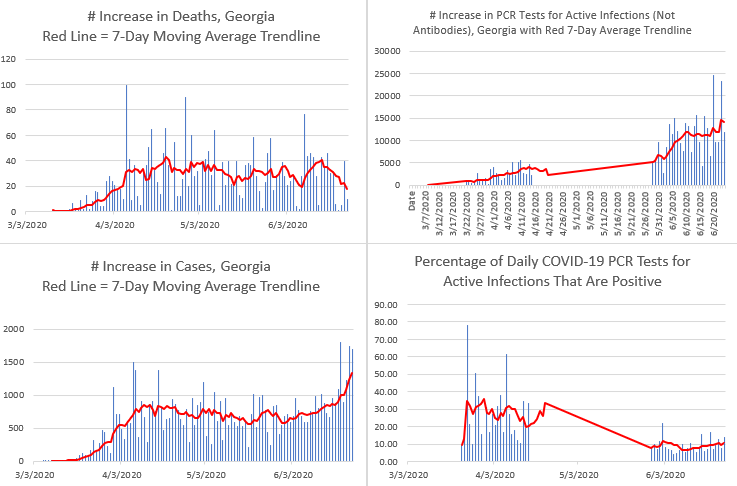
Dr. Jeffery Jones: “Below are graphs I made from data from the Georgia Department of Public Health’s daily COVID-19 data updates. The red lines represent trendline averages over the 7 prior days of increases in deaths, cases, tests, and positivity. There are usually daily fluctuations in these numbers, so trendlines help to show clearer patterns. Also note that these data are something like apples and oranges. Georgia now reports around 11,000 test results for active infections daily. Deaths, fortunately, have increases in the dozens or less. You can, however, compare the red trendlines for some insights. The number of deaths per day rose rapidly into April and then has fluctuated up and down since then. Cases went up rapidly in March, then began to come down to a plateau, and now have increased statewide to the highest daily increases of the pandemic.
But back to this question of whether daily increases in cases is linked to daily increases in testing. From April 16-May 28, Georgia strangely mixed antibodies testing (for past infections) with PCR testing (for active infections). So you will see that I left out these data because I don’t know how many of the daily increases were for the active virus or antibodies. Through June the state has increased testing with a plateau of about 11,000 test results per day since June 9. With more media attention to a rise in cases, new tests have jumped this week. So, for much of the latest rise in cases, testing was still at 11,000 daily. Overall in June, the number of cases has indeed gone up as testing has gone up, but in recent weeks the trendline for cases has gone up more sharply than the trendline for more testing.
Positivity: And that brings us to looking at the percentage of daily tests that are positive for active infection with SARS-CoV-2. In March and April, the percentage of people tested were far more likely to be positive because tests were scarce. The scarce available tests were used to screen people who had high risk factors and symptoms. The positivity rate peaked on April 7 at 61.6% of tests being positive. Then you can see this long stretch where the testing data was mixed up, and I have left out these data. On May 29 the state started publishing antibodies tests separate from PCR tests for active infections. There are a LOT more tests reported daily now. And as expected when you test more people, fewer of them are positive. However, you can see that the trendline shows the percentage of tests that are positive has been steadily rising.
So yes, some of the increase in cases probably is linked to more testing, but the increase in positivity in daily results points to increasing infections. Increased testing is likely showing a) a closer approximation to how many people are infected in Georgia in numbers we have not captured before and b) an increase in infected people as the state opens up. It isn’t one or the other in my opinion: it’s both.”
 Younger people are seeing less severe illnesses and our overall death count of 3 is low. Why should Bulloch County residents be concerned at all?
Younger people are seeing less severe illnesses and our overall death count of 3 is low. Why should Bulloch County residents be concerned at all?
Dr. Jeffery Jones: “This is also a good question with multiple answers. a) People of different ages do not live separately usually. We are a community. Children and young people with a mild case or even no symptoms may be infecting other, vulnerable members of their family and community. b) Cases from New York are now being reported of children who survived a COVID-19 infection with no symptoms who are now displaying health issues similar to Kawasaki disease. c) A study released in the past few weeks found that people -including young people- who had a mild case or even no symptoms now show signs of lung damage. In Georgia, the largest group of people infected with the SARS-CoV-2 coronavirus are now Georgians 18-29 years in age. While deaths in this age group have fortunately been few, that can change. This is a tricky virus. And there are negative outcomes other than death for young people that are possible: severe illness, isolation after diagnosis from work and loved ones, and long-term health issues we are not yet aware of. I know I am also not alone in worrying about the risk I pose when I visit my 80-year-old mother. My students tell me often that they do not worry about their own health that much: they worry about taking the virus to their grandparents or parents.”
What is the best way, as a community that we can respond without having to shut down the Bulloch County economy?
Dr. Jeffery Jones: “Other countries such as South Korea, Japan, New Zealand, etc. have been successful in largely controlling the pandemic in their countries. Then they have re-opened their economies. The CDC released guidelines for doing similar, but these have largely been ignored.
Some of these strategies, however, can work in Bulloch County such as everyone wearing a mask when in public. Respiratory masks (like N95) and surgical/medical masks (the common blue, pleated ones) have been shown in studies to protect healthcare workers from being infected with influenza, another disease, by their patients. Simple cloth masks offer inferior protection, but when almost everyone wears them it creates a synergy where virus transmission is reduced. Avoid crowds …and especially in enclosed spaces. Other countries have avoided returns to large-scale shutdowns through robust testing, contact tracing, and isolation of community members until they (and people exposed to them) no longer pose a risk of infecting others. They have then been able to close specific businesses or towns to deal with outbreaks rather than an entire state or country.”
In your estimation, what would indicate a dire need to order shelter in place countywide again?
Dr. Jeffery Jones: “This is a question for our political leaders, but again I would say that it comes down to whether we have the community systems in place to deal with rises in infections surgically via closure of specific businesses, schools, or social networks such as South Korea does, or are we in a situation where large numbers of the population refuse to follow basic safety guidelines such as social distancing and masks. We have evidence of how other communities and countries have come together through trust, clear messaging from leaders, and a prioritization of community/family over self to stop the spread and to then safely re-open. Even in these “success stories”, however, they are not done. These other communities and countries continue every day to have to employ these interventions and systems to deal with new cases. It isn’t a one-and-done effort but a long haul until we have a vaccine and/or cure.”




